Changes to the vaginal area are a common experience for many women, often occurring as a natural consequence of childbirth or the aging process. These changes can manifest as a feeling of looseness, known as vaginal laxity, sometimes accompanied by reduced sensation during intimacy or dissatisfaction with the area's appearance. For individuals seeking to address these concerns, vaginoplasty offers a surgical solution. This procedure is specifically designed to tighten the vaginal canal and its supporting structures, aiming to restore a feeling of firmness and support. Vaginoplasty serves a dual purpose: it can enhance physical function, potentially improving support and sensation, while also refining the aesthetic appearance of the vaginal opening, contributing positively to self-confidence and overall well-being. For those considering this specialized procedure, Istanbul, Turkey, has emerged as a recognized international destination, known for offering advanced medical care and specialized expertise in the field of genital aesthetic surgery. The decision to pursue vaginoplasty often arises from a desire to counteract the physical effects of significant life events like childbirth or aging, representing a step towards restoring personal comfort, function, and confidence rather than being solely about cosmetic alteration.
Table of Contents
1. Understanding Vaginoplasty: More Than Just Tightening 2. Could Vaginoplasty Be Right for You? Candidacy and Considerations 3. The Vaginoplasty Journey: What to Expect Before Surgery 4. Inside the Operating Room: The Vaginoplasty Procedure 5. Navigating Recovery: Healing After Vaginoplasty 6. Understanding the Risks and Ensuring SafetyUnderstanding the Risks and Ensuring Safety 7. Potential Benefits: Restoring Confidence and Function 8. Frequently Asked Questions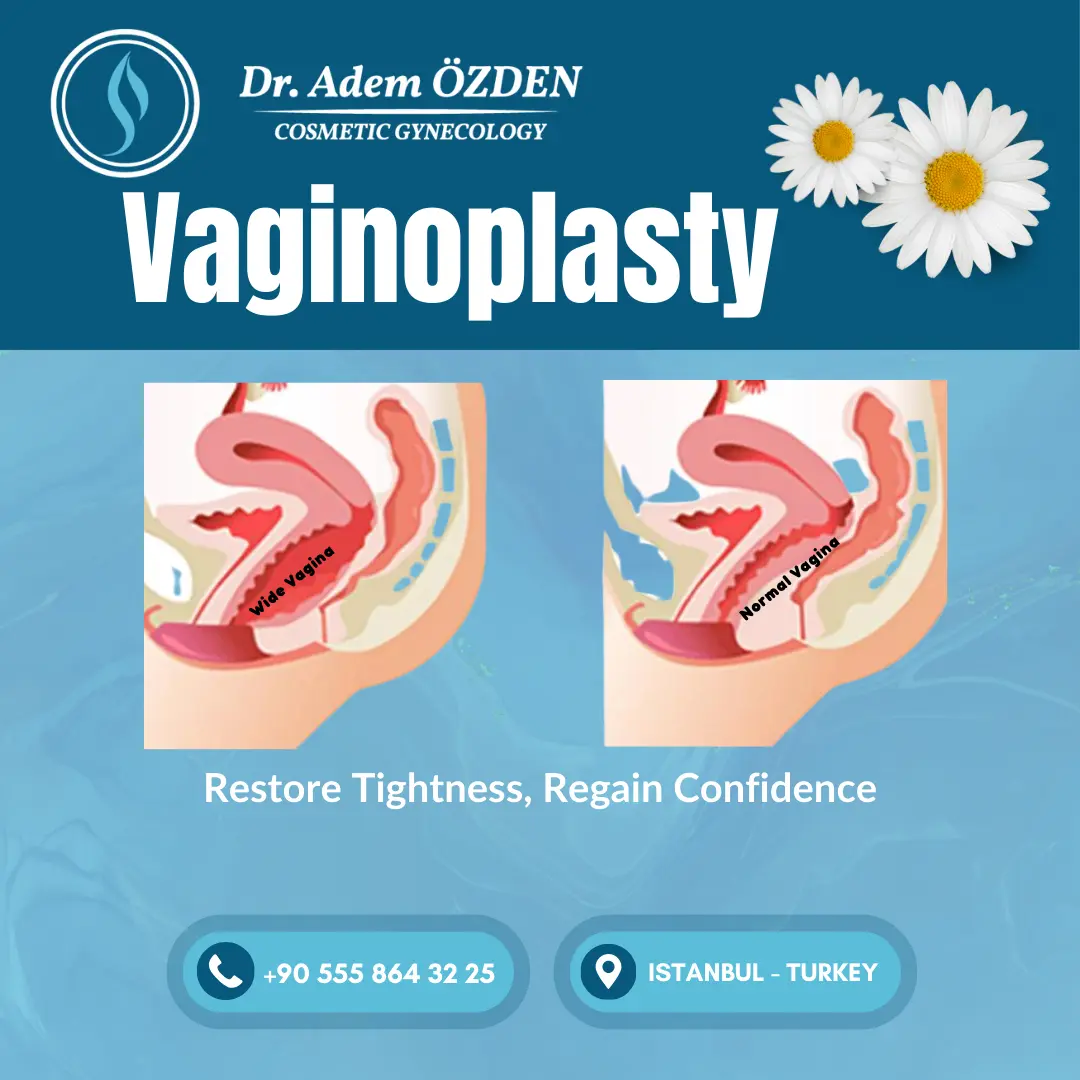
Understanding Vaginoplasty: More Than Just Tightening
Vaginoplasty is technically defined as a surgical procedure involving the reconstruction or repair of the vagina. Within the specialized field of genital aesthetics for women seeking enhancement after childbirth or due to aging, vaginoplasty primarily refers to procedures focused on tightening the vaginal canal and often the vaginal opening. Understanding the reasons behind vaginal changes provides context for the procedure. Vaginal delivery, particularly multiple births or the delivery of a large baby, can significantly stretch the vaginal tissues and potentially separate the underlying supportive muscles, such as the levator ani complex. Similarly, the natural aging process contributes to changes, involving a loss of tissue elasticity and shifts in hormonal balance, particularly decreased estrogen levels, which can affect tissue integrity. Explaining this anatomical basis helps clarify that feelings of laxity often have a physiological origin, validating patient concerns and illustrating how surgery aims to address these structural changes.
The objectives of vaginoplasty are typically twofold, encompassing both functional restoration and aesthetic improvement. Functionally, the surgery aims to restore vaginal tone by repairing and tightening the supportive muscles and tissues. This tightening can lead to increased friction during intercourse, potentially enhancing sensation for both the patient and their partner. It can also address practical concerns like tampons not staying in place or unwelcome sounds during physical activities. In some instances, strengthening the vaginal structures may contribute to improved pelvic floor support or help alleviate symptoms of mild stress urinary incontinence. Aesthetically, the procedure seeks to improve the appearance of the vaginal opening and external genital area, which can significantly enhance self-esteem and reduce feelings of self-consciousness.
It is important to distinguish vaginoplasty from other related genital aesthetic procedures. Labiaplasty specifically involves altering the size or shape of the labia minora (inner lips) or labia majora (outer lips). Perineoplasty focuses on repairing the perineum, the area between the vaginal opening and the anus, often addressing tears or laxity at the vaginal entrance. Clitoral hood reduction removes excess tissue covering the clitoris. While vaginoplasty addresses the internal vaginal canal, it can sometimes be performed in conjunction with these other procedures for a more comprehensive result. The term "vaginal rejuvenation" is a broader marketing term that can encompass any of these surgical procedures, as well as non-surgical treatments aimed at improving vaginal appearance or function. Clarifying the specific focus of vaginoplasty—internal tightening—helps manage expectations for those considering this particular surgery.
Contact Us Now For a Free Consultation
Get a quote and consultation for treatments from our expert doctors!
Could Vaginoplasty Be Right for You? Candidacy and Considerations
Individuals consider vaginoplasty for various reasons, primarily stemming from physical changes that impact their comfort, function, or self-perception. The most common driver is vaginal laxity experienced after childbirth, particularly following multiple deliveries, difficult births, or the birth of a large baby. The natural effects of aging, including the loss of tissue elasticity and hormonal shifts, are another frequent reason. Less commonly, significant weight fluctuations or inherent genetic factors might contribute to vaginal looseness. Specific symptoms prompting consideration often include decreased sexual satisfaction due to reduced friction or sensation, physical discomfort or irritation, a sensation of the vagina feeling too "open", or related concerns about appearance impacting self-esteem.
Determining suitability for vaginoplasty involves evaluating several factors. Generally, ideal candidates are individuals who:
- Experience vaginal laxity or related symptoms that are bothersome enough to seek correction.
- Are in good overall physical health, without major medical conditions that could increase surgical risks.
- Are non-smokers or are firmly committed to quitting smoking and all nicotine use well in advance of surgery and throughout the recovery period, as smoking significantly impairs healing.
- Possess realistic expectations regarding the potential outcomes, benefits, and limitations of the surgery. Understanding what the procedure can and cannot achieve is crucial for satisfaction.
- Are emotionally prepared for the surgical experience and the required recovery phase.
- Have ideally completed their family planning, as subsequent pregnancies and vaginal deliveries can potentially alter the surgical results over time. This factor makes the timing of the surgery an important discussion point, especially for younger individuals.
Certain conditions or circumstances may make vaginoplasty unsuitable or require careful evaluation. These potential contraindications include active genital infections, current pregnancy, certain untreated pelvic floor disorders, significant underlying medical problems that elevate surgical risks, unrealistic expectations about the outcome, or an inability to adhere to necessary post-operative care instructions. Smoking is a major contraindication due to its detrimental effects on wound healing. A very high Body Mass Index (BMI) might also be considered a relative risk factor due to potential healing complications.
Given these considerations, a comprehensive consultation with a qualified surgeon specializing in genital aesthetic procedures is essential. This consultation allows for a detailed discussion of the patient's specific concerns, goals, and complete medical history. It includes a physical examination to assess the degree of laxity and suitability for surgery. The surgeon will explain the proposed surgical plan, discuss the potential risks and benefits, outline the expected recovery process, and answer all patient questions thoroughly. This ensures the patient can make a fully informed decision based on a clear understanding of the procedure and its implications. Psychological readiness and aligned expectations are just as important as physical suitability for achieving a satisfactory outcome.
The Vaginoplasty Journey: What to Expect Before Surgery
Preparing for vaginoplasty involves several important steps, beginning with the initial consultation and extending through various pre-operative requirements. This preparation phase underscores that vaginoplasty is a significant surgical procedure requiring patient commitment and planning for optimal safety and results.
The consultation itself is a critical first step. During this meeting, the patient will have an in-depth discussion with the surgeon about their specific concerns, desired outcomes, and complete medical history. A physical examination will be performed to assess the vaginal anatomy and degree of laxity. The surgeon will then explain the recommended surgical approach, detailing the potential techniques, the expected benefits, the possible risks and complications, and the anticipated recovery process. This is also the time for the patient to ask any questions they may have to ensure full understanding. Obtaining informed consent, confirming the patient understands all aspects of the procedure before agreeing to it, is a mandatory part of this process.
Following the decision to proceed, the surgeon will provide specific pre-operative instructions. These typically include:
- Medical Clearance: Patients may need routine blood tests or other medical evaluations to confirm their fitness for surgery and anesthesia.
- Medication Management: Instructions will be given to stop taking certain medications and supplements that can increase bleeding risk, such as aspirin, non-steroidal anti-inflammatory drugs (NSAIDs like ibuprofen), blood thinners, vitamin E, and some herbal remedies, usually starting one to two weeks before surgery. Hormone therapy (like estrogen) may also need to be paused for a specified period before surgery.
- Smoking and Nicotine Cessation: Complete cessation of smoking, vaping, and all nicotine products is typically required for several weeks (often at least 3 months) before and after surgery due to nicotine's severe negative impact on blood flow and tissue healing. Nicotine testing may be performed to confirm compliance.
- Alcohol Restriction: Patients are usually advised to avoid alcohol consumption in the week leading up to surgery.
- Diet and Hydration: Specific instructions regarding eating and drinking will be provided, often involving a clear liquid diet the day before and fasting (nothing by mouth) after midnight. Maintaining good hydration in the days leading up is also important. Bowel preparation might be required the day before surgery to empty the bowels.
- Hygiene: Instructions may include showering with a specific antiseptic soap (like chlorhexidine gluconate - CHG) for a few days before surgery to reduce skin bacteria. Shaving the genital area should generally be avoided close to the surgery date unless specifically instructed.
- Logistical Arrangements: Planning for recovery is crucial. This includes arranging sufficient time off from work or other responsibilities (typically 1-2 weeks minimum, potentially more) , organizing transportation home after surgery, and ensuring a support person is available, particularly during the first few days of recovery. Preparing the home environment by stocking necessary supplies (like pads, comfortable clothing, cushions) and perhaps pre-making meals can ease the recovery process.
- Emotional Well-being: Acknowledging the emotional component of undergoing surgery is important. Utilizing support systems like family, friends, or therapists can be beneficial.
The comprehensive nature of these preparations highlights that vaginoplasty requires careful planning and patient participation to ensure the best possible outcome.
Inside the Operating Room: The Vaginoplasty Procedure
The vaginoplasty procedure itself is performed in a sterile surgical setting, typically taking between one to two hours for cases focused on vaginal tightening, although the exact duration can vary based on the extent of correction needed and whether other procedures are combined.
Patients are usually placed under general anesthesia for vaginoplasty, meaning they will be completely asleep and unaware during the surgery, ensuring comfort and stillness. In some select cases, local anesthesia combined with intravenous sedation might be used. Throughout the operation, vital signs such as heart rate, blood pressure, and oxygen levels are continuously monitored for safety.
The surgical steps for vaginal tightening generally involve the following, explained in accessible terms:
- Incisions: The surgeon makes precise incisions, usually within the lining of the vagina (vaginal mucosa). Often, these incisions are placed along the posterior (back) wall of the vagina. An alternative approach involves incisions along the sides (lateral colporrhaphy). The location and length depend on the specific areas requiring tightening.
- Muscle and Tissue Repair: This is the core element of the procedure. The surgeon identifies the underlying vaginal muscles that may have become stretched or separated (such as the levator ani muscles, bulbocavernosus, and transversus perinealis). These muscles are then carefully tightened and brought closer together using strong sutures. This internal restructuring restores support and effectively reduces the overall diameter of the vaginal canal.
- Removal of Excess Tissue: Any redundant or stretched vaginal lining (mucosa) resulting from the tightening process is carefully measured and excised.
- Closure: The incisions made in the vaginal lining are meticulously closed with sutures. Frequently, these sutures are dissolvable, meaning they will be absorbed by the body over time and do not require manual removal. This simplifies one aspect of the recovery process. As part of the closure, the vaginal opening (introitus) may also be surgically narrowed if needed.
While specific techniques like posterior or lateral colporrhaphy exist, the optimal approach is determined by the surgeon based on the individual patient's anatomy and the specific nature of their concerns. The procedure may also be combined with a perineoplasty to specifically repair the vaginal opening and perineal body. The emphasis is on achieving noticeable and consistent results through meticulous surgical skill.
Immediately following the surgery, sterile packing may be placed inside the vagina to support the tissues and manage initial bleeding. A temporary urinary catheter to drain urine and small surgical drains to remove excess fluid might also be used, depending on the surgeon's preference and the specifics of the operation.
Navigating Recovery: Healing After Vaginoplasty
The recovery period following vaginoplasty is a crucial phase that requires careful management and patient adherence to instructions for optimal healing and results. Recovery is an active process, not just passive waiting, and involves several stages with specific guidelines and expectations.
Initial Hospital Stay and Discharge:
For vaginoplasty focused on tightening, the hospital stay is often relatively short. Many patients can be discharged the same day (outpatient) or after one to two nights of observation. Longer stays might be necessary for more complex cases or if combined with other major procedures. Before discharge, the medical team ensures the patient is medically stable, pain is adequately managed, and provides detailed instructions for home care. Arrangements for a responsible adult to drive the patient home and provide initial support are essential.
Immediate Post-Operative Phase (First Few Days to Week 1-2):
- Pain and Discomfort: Soreness, swelling, and bruising in the genital area are expected and typically peak in the first few days. Pain is generally manageable with prescribed pain medications, transitioning to over-the-counter options as discomfort subsides. Pain should gradually decrease; any significant increase warrants medical attention.
- Packing, Catheter, Drains: Vaginal packing, if used, is typically removed within a day or two, often before discharge. Urinary catheters and surgical drains are also usually removed before going home or at the first follow-up visit.
- Bleeding and Discharge: Light vaginal bleeding or spotting is normal for the first few days or weeks. A brownish or yellowish discharge may also occur as tissues heal. Sanitary pads should be used; tampons are strictly prohibited during the initial healing period.
- Rest and Mobility: Rest is paramount during the first week or two. However, gentle, short walks are encouraged early on to promote circulation and prevent blood clots. Prolonged sitting can be uncomfortable; using a donut cushion or similar support can help relieve pressure. Wide leg movements should be avoided.
Early Recovery Phase (Weeks 2-6):
- Activity Restrictions: Strenuous activities, including heavy lifting (typically over 10 pounds), vigorous exercise, running, cycling, and swimming, must be avoided for approximately 4-6 weeks, or as advised by the surgeon.
- Return to Work: Depending on the nature of the job and individual healing progress, returning to work may be possible within 1-2 weeks for sedentary roles. More physically demanding jobs may require 4-8 weeks off.
- Sexual Activity and Tampons: Sexual intercourse and the use of tampons remain restricted for approximately 6 to 8 weeks, or until the surgeon confirms adequate healing.
- Hygiene: Maintaining meticulous hygiene is crucial to prevent infection. This involves keeping the surgical area clean and dry, following specific washing instructions (gentle cleansing, patting dry, wiping front to back after using the toilet). Baths, hot tubs, and swimming pools should be avoided until incisions are fully healed. Wearing loose-fitting cotton underwear and clothing is recommended.
- Swelling and Sensation: Swelling continues to gradually decrease but may persist to some degree for several weeks or even months. Temporary numbness, tingling, or altered sensation in the area is common as nerves recover. Itchiness can also occur as part of the healing process.
- Diet: Continuing a diet rich in fiber and fluids helps prevent constipation, which could cause straining and discomfort. Stool softeners may be recommended.
Longer-Term Healing and Results (Beyond 6-8 Weeks):
- Activity Resumption: Most normal activities, including exercise and sexual intercourse, can typically be gradually resumed around 6-8 weeks post-surgery, pending surgeon clearance. It's important to start gently and listen to the body.
- Final Outcome: While significant improvement is noticeable earlier, the final results take time to fully manifest. Residual swelling can take 4-6 months, or sometimes up to a year, to completely resolve, and tissues need time to soften and settle. Scarring from vaginoplasty is primarily internal and usually not visible externally. Full return of normal sensation can also take several months.
- Vaginal Dilation: Unlike vaginoplasty for vaginal creation (often performed for gender affirmation), which requires a rigorous and often lifelong dilation schedule to maintain canal depth and width, routine, long-term dilation is less commonly mandated after vaginoplasty solely for tightening in cisgender women. However, some surgeons may recommend using dilators for a specific period post-operatively to ensure the vaginal opening and canal remain adequately open during healing. It is crucial for patients to follow the specific dilation protocol (if any) provided by their individual surgeon.
- Follow-Up Care: Attending all scheduled follow-up appointments is essential for monitoring healing progress, addressing any concerns, and receiving clearance for resuming activities.
Understanding the Risks and Ensuring SafetyUnderstanding the Risks and Ensuring Safety
While vaginoplasty is generally considered safe and often yields high patient satisfaction when performed by experienced surgeons, it is essential for prospective patients to understand that, like any surgical procedure, it carries potential risks and complications. Transparency about these risks is crucial for making an informed decision.
General risks inherent to most surgeries apply, including the possibility of excessive bleeding (hemorrhage) during or after the procedure, infection at the surgical site, adverse reactions to anesthesia, and the formation of blood clots in the legs (deep vein thrombosis or DVT) which could potentially travel to the lungs (pulmonary embolism or PE).
In addition to these general risks, there are potential complications specific to vaginoplasty:
- Pain: While post-operative pain is expected and manageable, some individuals may experience persistent pain or the development of dyspareunia (painful sexual intercourse).
- Bleeding/Hematoma: Bleeding beyond normal spotting or the formation of a hematoma (a collection of blood under the skin), may occur and might require intervention.
- Infection: Despite preventative antibiotics, surgical site infections can develop, potentially requiring further treatment. Poor hygiene can increase this risk.
- Scarring: Although incisions are mostly internal, excessive or thickened scar tissue could potentially form, although significant visible scarring is uncommon.
- Sensation Changes: Temporary or, rarely, permanent numbness, decreased sensation, or altered/unpleasant sensations (dysesthesia) in the vaginal or clitoral area can occur due to nerve irritation or damage during surgery.
- Stenosis/Stricture: Excessive narrowing (stenosis) of the vaginal canal or opening (introitus) can occur, potentially making intercourse, tampon use, or even pelvic exams difficult or painful.
- Wound Healing Problems: Issues such as delayed healing, wound separation (dehiscence), or, rarely, tissue necrosis (death of skin or tissue flaps due to compromised blood supply) can occur, particularly in smokers or those with certain medical conditions. Hypergranulation tissue (excessive healing tissue) can sometimes form in areas healing by secondary intention.
- Fistula: A rare but serious complication is the formation of a fistula, an abnormal passageway between the vagina and the rectum (rectovaginal fistula) or the bladder/urethra (vesicovaginal/urethrovaginal fistula). This typically requires corrective surgery.
- Urinary Issues: Changes in the urinary stream (like spraying), temporary difficulty urinating, or, very rarely, injury to the urethra or development of incontinence can occur.
- Unsatisfactory Results: Patients may be dissatisfied with the aesthetic outcome, feel the vagina is too tight or still too loose, or experience asymmetry. Revision surgery may sometimes be necessary.
Fortunately, the likelihood of these complications can be significantly reduced. Key factors in ensuring safety include careful patient selection (choosing candidates who are healthy and have realistic expectations), the surgeon's expertise and meticulous surgical technique, and the patient's strict adherence to all pre-operative and post-operative instructions. Studies suggest that surgeon experience, particularly the number of procedures performed, correlates with lower rates of certain complications, emphasizing the importance of choosing a highly qualified and experienced surgeon. Patient compliance with post-operative care, such as activity restrictions and hygiene protocols, also plays a vital role in minimizing risks like infection and wound breakdown.
Potential Benefits: Restoring Confidence and Function
Vaginoplasty surgery offers a range of potential benefits for individuals seeking to address concerns related to vaginal laxity. These benefits often extend beyond the physical changes, positively impacting emotional well-being and overall quality of life.
The primary physical outcome is enhanced vaginal tone and tightness. The surgical repair of underlying muscles and removal of excess tissue results in a narrower, firmer vaginal canal and opening. This restoration of anatomical support can lead to several functional improvements. Many patients report improved sexual function and satisfaction, often attributed to increased friction and potentially heightened sensation during intercourse for both partners. High patient satisfaction rates are often reported following the procedure. However, it is important to maintain realistic expectations, as sexual response is complex and influenced by many factors beyond vaginal anatomy; heightened sensation or improved orgasm cannot be guaranteed solely by the surgery.
Beyond sexual function, patients often experience increased physical comfort. Issues associated with laxity, such as irritation from clothing, difficulty keeping tampons in place, or embarrassing sounds during exercise or intimacy, can be alleviated. In some cases, the improved support provided by vaginoplasty may also help reduce symptoms of mild stress urinary incontinence.
Aesthetically, the procedure can enhance the appearance of the vaginal opening and surrounding vulvar area, leading to a more youthful or desired look. This combination of physical and functional improvements often translates into significant psychological benefits. Many individuals report a substantial boost in self-esteem and confidence, feeling more comfortable and positive about their bodies, particularly in intimate situations. Ultimately, these combined effects can lead to an improved overall quality of life. The benefits often create a positive cycle where physical restoration leads to functional improvement, enhancing psychological well-being and satisfaction.
